By Adrienne Dellwo
Table of Contents
- Is Fibromyalgia an Autoimmune Disease?
- Autoimmunity
- Neuroinflammation
- Small-Fiber Neuropathy
- Frequently Asked Questions
Fibromyalgia (FM) may be an autoimmune disease, where your immune system attacks healthy cells by mistake. For years, the evidence seemed to point away from that. This issue is still far from decided, but opinion may be swaying back toward autoimmunity.
Some research suggests FM may be an autoimmune disease involving neuroinflammation, an inflammatory response within the brain and spinal cord, and small-fiber neuropathy, which is weakness and pain from nerve damage.1
That hypothesis isn’t getting widespread acceptance in the medical community, though.
This article looks at what this research says; the evidence for autoimmunity, neuroinflammation, and small-fiber neuropathy; why not all inflammation is created equal; and why these findings—if accurate—are important.
Is Fibromyalgia an Autoimmune Disease?
For decades, fibromyalgia’s very existence was controversial. But not anymore. Early on, some doctors who believed in FM classified it as “arthritis-like.”2
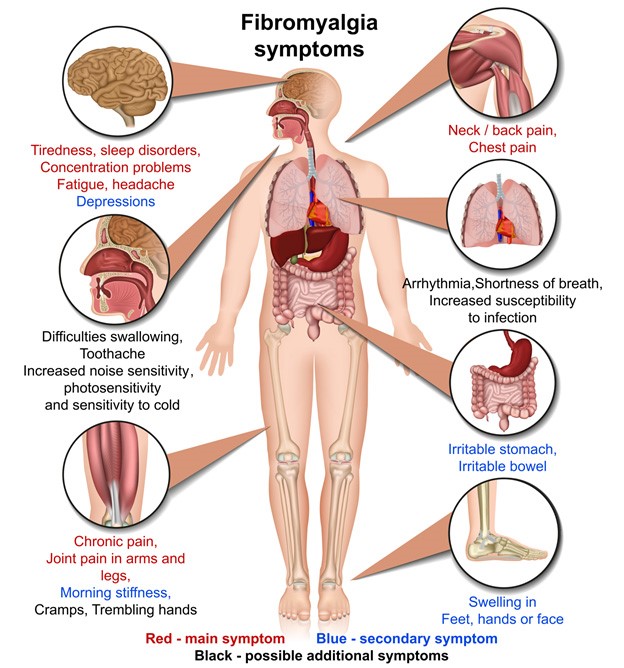
Many medical experts suspected autoimmunity because of the condition’s similarities to known autoimmune diseases such as lupus, Sjögren’s syndrome, rheumatoid arthritis, and multiple sclerosis.
However, early research failed to turn up the hallmarks of autoimmune disease, including:
- Damage from the immune system attack
- Inflammation as part of the immune and healing processes
- Autoantibodies (immune system proteins that target a part of your body)
What Is Autoimmunity?
Autoimmunity is an immune system turned against its body. Your immune system mistakes a healthy type of cell or tissue in your body for a dangerous pathogen, like a virus or bacterium. It then attacks and tries to destroy the target. This leads to tissue damage, inflammation, and other symptoms.
Later, FM was considered a pain condition that was believed to be neurological or neuroimmune. The term central sensitivity syndrome developed as an umbrella term for FM and related illnesses, including myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), irritable bowel syndrome (IBS), and migraine.
Now, FM is seen as a complex, multi-symptom illness. What’s more, some evidence suggests it actually isn’t missing those hallmarks of autoimmunity:1
- Damage? Yes, small-fiber neuropathy.
- Inflammation? Yes, in the brain and nerves of the spinal cord (central nervous system).
- Autoantibodies? Yes, several of them.
What You Need to Know About the Nervous System
Autoimmunity
Fibromyalgia has always borne a striking resemblance to autoimmune diseases. Research published in 2019 laid out the many factors they have in common:1
- They’re often triggered by trauma and infection.
- Various pathogens may increase your risk (Epstein-Barr virus, herpes simplex virus, hepatitis C).
- They can develop soon after vaccination, silicone breast implantation, or mineral oil injection.
- They’re more common in women.
- They involve genetic differences known to predispose you to autoimmunity.
- They often occur alongside other autoimmune diseases.
- Evidence shows activation of the adaptive immune system.
Autoinflammatory vs. Autoimmune: Two Immune Systems
Autoantibodies
Researchers believe they may have found the smoking gun of autoimmunity in FM as well. They discovered that several autoantibodies were unusually high in people with FM, including those for:
- Serotonin: A neurotransmitter (chemical messenger) and hormone known to be dysregulated in FM1
- Gangliosides: A type of molecule in the brain linked to several neurodegenerative conditions, including Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS)3
- Phospholipids: Molecules that make up protective barriers around cells and regulate certain cellular processes
- Smooth muscle: Muscles located in organs, under involuntary control
- Striated muscle: Skeletal muscles, under voluntary control
- Moisture-producing glands: The same autoantibodies as in Sjögren’s syndrome which affect moisture-producing glands in the mucous membranes that line organs and the inside of your body
- Thyroid gland: The same autoantibodies as in Hashimoto’s thyroiditis, an autoimmune thyroid disease1
None of these were found in every person with FM. Rates ranged from about 19%4 to 73%.1
Gangliosides may be an important aspect of FM autoimmunity. They’re believed to be involved in small-fiber neuropathy.5
| Autoantibody Rates, FM Studies | |
|---|---|
| Serotonin | 73% |
| Gangliosides | 71% |
| Phospholipids | 54% |
| Smooth muscle | 55% |
| Striated muscle | 40% |
| Sjögren’s syndrome antibodies | 32% |
| Thyroid gland | 19% |
*Among those with Sjögren’s syndrome
Giving Fibromyalgia to Mice
In a groundbreaking 2021 study, researchers took antibodies (immunoglobulin G, IgG) from people with FM and injected them into mice. The mice then:6
- Developed hypersensitivity to pain and cold
- Became less active
- Lost paw grip strength
- Lost nerve fibers in the skin
Researchers say the FM IgG appeared to target white-matter brain cells (glia), gray-matter brain cells (neurons), and certain nerve fibers. This shows how immune system activity can cause neurological symptoms.
The ability to transfer FM like this is nothing short of revolutionary. On top of providing evidence about what’s causing symptoms, it could point to new diagnostic tests and treatments.6
How the Immune System Works
Diagnosis and Treatment
If more research validates findings of autoimmunity in fibromyalgia, it could lead to diagnostic tests. For a condition that’s currently a diagnosis of exclusion, that’s an important change.
Many immunosuppressive drugs for autoimmune diseases are already on the market. That greatly expands treatment options, especially since the drugs could be used off-label right away.
It remains to be seen whether current immunosuppressants are safe and effective for FM.
Neuroinflammation
Several studies have now confirmed neuroinflammation in fibromyalgia. Some also have looked at where it is in the brain and what may be driving it.
Inflammation is a complex immune response to injury and infection. It’s a necessary function. But when it becomes chronic, inflammation causes tissue damage. It’s especially harmful in the nervous system.7
:max_bytes(150000):strip_icc():format(webp)/Autoimmunity-neuroinflammation-in-fibromyalgia-5197944-final-06cac9e71094433f91d57525df899944.jpg)
The nervous system and immune system work together to create neuroinflammation. FM research links several cells and one molecule to the process.
Neurological components include:
- Microglia: A type of cell that’s part of the nervous system’s dedicated immune system7
- Astrocytes: Cells of the brain and spinal cord involved in information processing and implicated in neurodegenerative disease8
- Oligodendrocytes: White-matter cells that form myelin sheaths around nerves and regulate neuronal circuits7
- Brain-derived neurotrophic factor (BDNF): A key molecule involved in learning and memory, also tied to aging and brain-related disease9
Immune system components include:
- Mast cells: A type of white blood cell that helps keep the immune system in balance7
- Chemokines: Immune cells that attract white blood cells to sites of infection10
- Pro-inflammatory cytokines: Immune system proteins that drive the inflammatory response11
- Interleukins: Proteins that regulate immune response10
- Tumor necrosis factor alpha (TNFα): A type of cytokine involved in inflammation and cell death9
- Macrophages: Tissue resident immune cells usually found at the site of infection
- T-cells: Specialized immune cells that target proteins identified (or misidentified) as foreign12
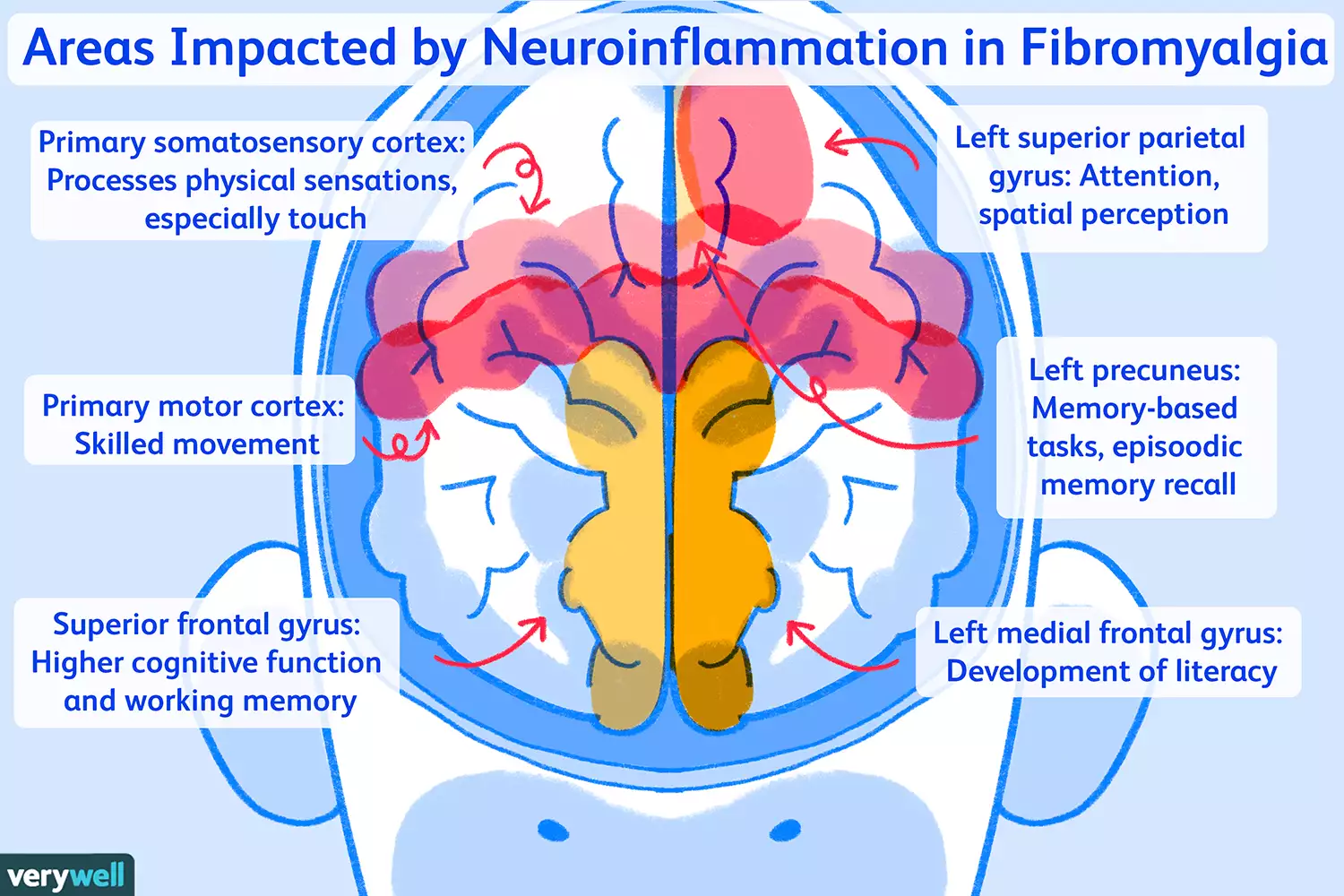
A 2021 study looked at where brain inflammation is in FM.13 Researchers found several areas with abnormal inflammation compared with healthy people in the control group.
Some of these areas play roles in functions that are often dysregulated in people with FM. They include:13
- Primary somatosensory cortex: Processes physical sensations, especially touch
- Primary motor cortex: Skilled movement
- Superior frontal gyrus: Higher cognitive function and working memory
- Left superior parietal gyrus: Attention, spatial perception
- Left precuneus: Memory-based tasks, episodic memory recall
- Left medial frontal gyrus: Development of literacy
They also found abnormally low inflammation-related activity in the:13
- Medulla: Relays messages between the brain and spinal cord, regulates cardiovascular and respiratory systems (heart and lungs)
- Amygdala: Drives the stress and fear response (fight-or-flight)
- Left superior temporal gyrus: Language processing, remembering what you’ve just heard
Neuroinflammation in the amygdala, left medial frontal, and left superior parietal gyri was associated with higher pain scores. Neuroinflammation in the left amygdala, left medial frontal, and left superior frontal gyri was associated with higher stress responses, which included measures of fatigue, tension, frustration, depression, somatization, and aggression.13
How Your Brain Works
A Different Type of Inflammation
Neuroinflammation has different effects than “typical” inflammation in the joints and soft tissues. Typical inflammation causes pain in many conditions, such as arthritis and multiple sclerosis.
When tissues expand beyond their normal size, they cause pain by putting pressure on surrounding structures. Arthritic fingers hurt because they’re inflamed.
Neuroinflammation doesn’t cause the same issues. Instead, it causes neurological problems that lead to neurological symptoms.
FM pain is believed to come from central sensitization, which is a heightened response to pain in the central nervous system. Research suggests neuroinflammation is behind central sensitization.14
So, regardless of neuroinflammation, your FM pain isn’t caused by tissue inflammation and therefore can’t be treated in the same way.
Diagnosis and Treatment
Inflammatory markers for fibromyalgia tend to be slightly elevated. But the cells and molecules involved in the neuroinflammation of FM may provide new diagnostic markers to look for.
Drugs that suppress microglia and astrocytes may be useful for treating neuroinflammation. They include:
- Low-dose naltrexone (LDN)
- Diamox (acetazolamide)
- Trental/Pentoxil (pentoxifylline)
- Zirgan (ganciclovir)15
- Rifadin (rifampin)16
- Enbrel (etanercept)17
- Precedex (dexmedetomidine)18
- Delsym/Robitussin (dextromethorphan)19
- Propentofylline (an experimental drug)
- Dynacin/Minocin/Solodyn (minocycline)
- Cannabidiol (CBD)9
- P2X7R inhibitors (experimental drugs)20
Other existing treatments for neuroinflammation include:
- Tricyclic antidepressants, including amitriptyline and nortriptyline21
- Low-dose corticosteroids
- Nutritional supplements, including vitamin B12
- Hormonal supplementation, including oxytocin, human growth hormone, and human chorionic gonadotropin22
Several other drugs are under development for neuroinflammation, most of them developed as potential Parkinson’s disease treatments. Anti-inflammatory drugs are often prescribed for neuroinflammatory disease as well. However, they’ve historically been considered ineffective for FM pain.
Small-Fiber Neuropathy
Small-fiber neuropathy (SFN) is nerve damage that’s only in the small sensory nerves of the skin.23 It’s probably best known in relation to type 2 diabetes.
As in FM, the pain comes and goes and is described as:24
- Stabbing
- Burning
- Tingling
- Itchy
Also like FM, SFN involves the abnormal pain types hyperalgesia and allodynia. Hyperalgesia makes your pain signals more intense, basically “turning up the volume” of pain. Allodynia makes things hurt that shouldn’t, like a loose waistband or a hand rubbing lightly against your skin.24
The 8 Types of Fibromyalgia Pain
SFN and fibromyalgia also have these symptoms in common:24
- Pain triggered by heat or cold
- Urinary problems
- Bowel problems
- Periodic rapid heartbeat
- Dry eyes and/or mouth
- Abnormal sweating
- Orthostatic intolerance (dizziness from a sharp drop in blood pressure upon standing)
FM research suggests some damaged nerves are part of anti-inflammatory processes. That provides another explanation for neuroinflammation.1
Typical SFN vs. Fibromyalgia SFN
In most SFN, pain begins in the feet and then moves upward. It’s been thought that only a small percentage of SFN begins with body-wide pain.24 The association between SFN and FM, which by definition includes body-wide pain, could change that belief.
Diagnosis and Treatment
The typical diagnostic test for SFN is a skin punch biopsy. A small amount of skin is removed with a circular tool and examined under a microscope. The focus is on nerve fiber density in the skin.
SFN is treatable, and small nerves continue to grow throughout life. That means they can repair damage.25
Standard SFN treatments are already heavily used for fibromyalgia. They include:
- Anti-seizure medications: Lyrica (pregabalin), Neurontin (gabapentin)
- Serotonin-norepinephrine reuptake inhibitors: Cymbalta (duloxetine), venlafaxine
- Tricyclic antidepressants: Amitriptyline, nortriptyline, desipramine
In a pilot study, treatment with intravenous immunoglobulin (IVIg) has been shown to improve SFN in FM. This treatment is known to be effective against autoimmune-related neuropathy. Biopsies confirmed that nerves showed less damage after treatment.26
Ganglioside autoimmunity may suggest treatment options as well. Gangliosides are suspected of being involved with diabetes-related small-fiber neuropathy. Some early animal research has suggested that ganglioside-targeted treatments may improve neuropathic pain.5
Currently, researchers are working on drugs called ganglioside GM3 synthase inhibitors.27 Evidence suggests that these may work as both oral medication and topical treatments.5
Summary
Research has uncovered evidence that FM is an autoimmune disease. Neuroinflammation and small-fiber neuropathy appear to be important elements of it. Autoantibodies could provide diagnostic markers for FM. Immunosuppressants may be treatment options. Neuroinflammation and SFN also offer potential diagnostic markers. Existing treatments are on the market. Some experimental drugs are in the works as well.
Reference<https://www.verywellhealth.com/autoimmunity-neuroinflammation-in-fibromyalgia-5197944